MALNUTRITION IN INDIA
2020 NOV 16
Mains >
Social justice > Health > Nutrition
WHY IN NEWS:
- India celebrates the first week of September 2020 as National Nutrition Week and dedicates the entire month for Nutrition related campaigns and activities by the Food and Nutrition Board
BACKGROUND:
- Malnutrition refers to deficiencies, excesses or imbalances in a person’s intake of energy and/or nutrients.
- The term malnutrition addresses 3 broad groups of conditions:
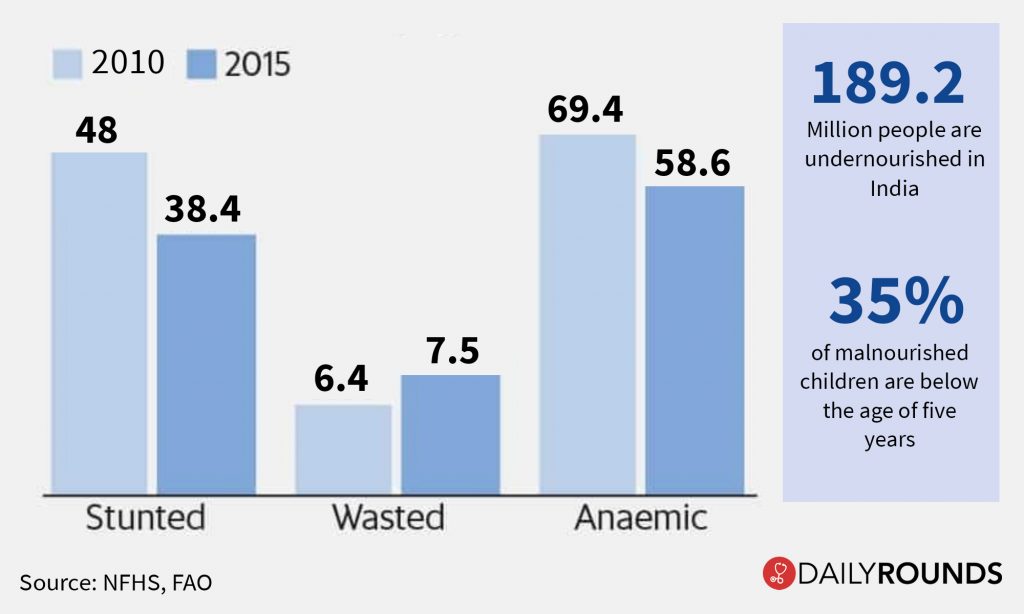
- Under nutrition: which includes wasting (low weight-for-height), stunting (low height-for-age) and underweight (low weight-for-age).
- Micronutrient-related malnutrition: which includes micronutrient deficiencies (a lack of important vitamins and minerals)
- Overweight: Obesity and diet-related non-communicable diseases (such as heart disease, stroke, diabetes and some cancers).
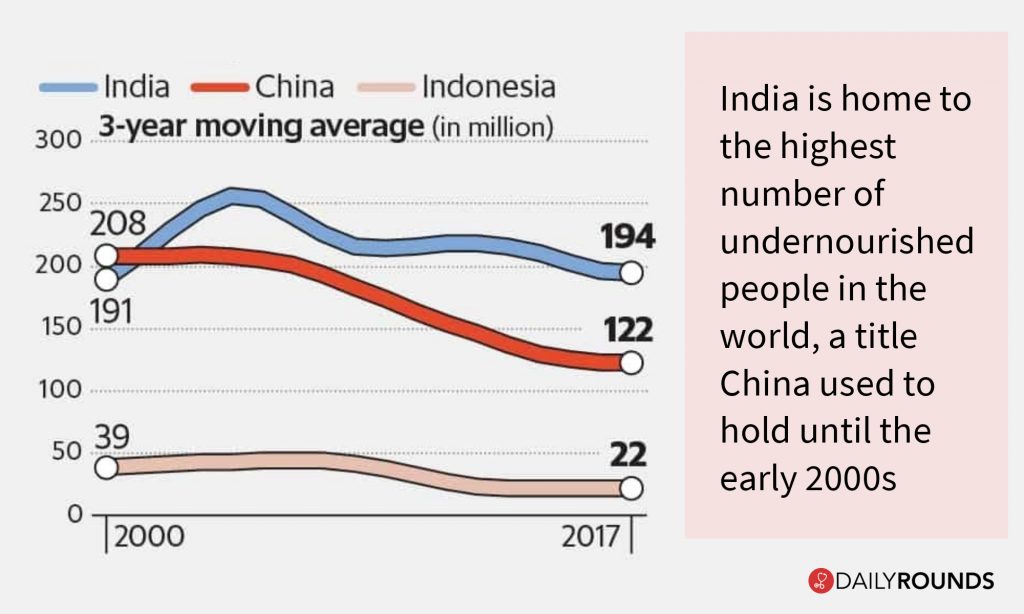
- India is home to the most number of malnourished children all across the world.
|
Hidden hunger occurs when the quality of food people eat does not meet their nutrient requirements, so the food is deficient in micronutrients such as the vitamins and minerals that they need for their growth and development.
|
- 14 percentage of India’s population is undernourished, according to ‘The State of Food Security and Nutrition in the World, 2020’
- Bihar and Uttar Pradesh have the highest number of malnourished children
- As per Global Hunger Index (GHI) 2019, India has been ranked 102 out of the qualifying 117 countries
- According to UNICEF report, over 80 per cent adolescents in India suffer from Hidden hunger
- Levels of anaemia among women and girls has stagnated over the last decade from 55.3% in NFHS-3 to 53% in NFHS-4
- The prevalence of obesity among 5 to 19-year-old Indian children, ranged between 3.6% and 11.7%. It is predicted that by 2025 there will be 17 million obese children in India
REASONS FOR HIGH PREVALENCE OF MALNUTRITION:
- Malnutrition occurs as a complex interplay among various factors such as:
- Poverty:
- It affects the availability of adequate amounts of nutritious food for the most vulnerable populations.
- Feeding habits
- Lack of awareness of nutritional qualities of food, irrational beliefs about food, inappropriate child rearing and feeding habits all lead to under nutrition in the family.
- Changing food patterns:
- Food consumption patterns have changed substantially in India over the past few decades, which has resulted in the disappearance of many nutritious local foods, for example, millets.
- Prevalence of infectious disease:
- Infections like malaria and measles or recurrent attacks of diarrhoea may precipitate acute malnutrition and aggravate the existing nutritional deficit.
- Metabolic demands for protein are higher during infections and the child may take in less food either due to reduced appetite or due to food restrictions by the mother. Thus leading to malnutrition
- Poor implementation of government policies:
- Government policies to improve nutritional security such as ICDS are poorly implemented.
- Monoculture agricultural practice:
- It has led to the over-emphasis on cereals and hence low production nutritious crops such as millets, pulses and horticultural crops.
- Poor sanitation:
- Lack of pure drinking water and poor sanitation leads to spread of diseases which lead to acute malnutrition.
- Gender inequality:
- Early marriages, less gap in pregnancies, malnourished pregnant girl, prevalence of anaemia adversely affects the nutritional status of the mother >> A malnourished mathoer will give birth to low birth weight baby
- Patriarchal character of society:
- Inequitable distribution of food in the family. In most of the poor households, women and preschool children especially girls receive less food than the economically active male members
- Social exclusion:
- Nutrition vulnerabilities are compounded by differentials in socio economic status and vary by vulnerable community groups such as SC, ST, minorities and others
- Migration:
- Seasonal migrations have long been a livelihood strategy for the poorest households in India.
- Migration in certain cases result in temporary and poor living condition, lack of access to PDS etc. >> which in turn lead to malnutrition
- Disasters:
- For instance coronavirus pandemic contributed to food shocks and worsen the situation further
- Floods and Droughts disrupt food supply chain and hence result in lower intake. Ex: Assam flood of 2020
- Intergenerational cycle of under-nutrition
- Intergenerational cycle of under-nutrition is often perpetuated, with a high incidence of babies born with low birth weight, more susceptible to infections, more likely to experience growth failure, reflected in high levels of child under-nutrition and anaemia.
- This intergenerational cycle of under-nutrition is accentuated by multiple deprivations related to poverty, social exclusion and gender discrimination.
GOVT INITIATIVES:
- Legislative measures :
- The National Food Security Act (NFSA), 2013:
- Aims to ensure food and nutrition security for the most vulnerable through making access to food a legal right.
- Maternity Benefit (Amendment) Act 2017:
- The amended act has increased the maternity benefits from 12 weeks to 26 weeks
- This is in line with the recommendation of the World Health Organisation which mentions that children should be exclusively breastfed by the mother for the first 24 weeks. Thus it will aid in improving survival rates of children and healthy development of both mother and child.
- Policies and schemes:
- Pradhan Mantri Matru Vandana Yojana (PMMVY):
- It is a maternity benefit programme which includes conditional cash transfers to pregnant women in their bank account directly to meet enhanced nutritional needs and partially compensate for wage loss.
- Integrated Child Development Scheme:
- It is a comprehensive programme for providing supplementary nutrition, immunization and pre-school education to the children
- National Nutrition Strategy (NNS):
- It was launched by NITI Aayog in 2017 to ensure that every child, adolescent girl, and woman attains optimal nutritional status - especially those from the most vulnerable communities.
- National Nutrition Mission:
- To enable integration of nutrition-related interventions cutting across sectors like women and child development, health, food and public distribution, sanitation, drinking water, and rural development.
- Mid-Day Meal Scheme:
- It is a school meal programme designed to better the nutritional standing of school-age children nationwide.
- The programme supplies free lunches on working days for children in primary and upper primary classes
- National Health Mission:
- The mission envisages achievement of universal access to equitable, affordable and quality health care services
- It has components for the prevention and reduction of anaemia in women
- National Policy for Children, 2013
- It aims to protect and encourage the rights of the children to survival, health, nutrition, education, development, protection and participation
- Swachh Bharat including Sanitation and the National Rural Drinking Water Programme
- State level-initiatives:
- Rajasthan Government launched Indira Gandhi Matritva Poshan Yojana to provide a cash transfer of ?6,000 to the mother for the birth of the second child.
WAY FORWARD:
- Decentralised approach
- Strengthen the ownership of Panchayati Raj institutions and urban local bodies over nutrition initiatives. This is to enable decentralised planning and local innovation along with accountability for nutrition outcomes
- Governance reforms:
- Convergence of state and district implementation plans for ICDS, NHM and Swachh Bharat
- Focus on the most vulnerable communities in districts with the highest levels of child malnutrition
- Service delivery models based on evidence of impact.
- Focussing on primary health care:
- Improving the primary health centres and other health care services in the rural areas will definitely improve the nutrition profile of women and children.
- Establish new mechanisms, such as National Nutrition Councils, for:
- Developing coherent nutrition policies
- Ensuring an integrated approach
- Raising nutrition as a priority
- Widening the agenda for nutrition.
- Social campaign for attitudinal change:
- Government should coordinate with civil society groups to launch mass campaigns on delaying marriage of girls, ensuring gender parity within families, need and benefit of proper sanitation facilities and balanced diet.
- Community led approach:
- Building a strong consensus at national and local levels about the importance of nutrition as an investment in the country’s future, rather than as a welfare expenditure
- Using community volunteers on a huge scale, to cut costs, involve and empower local people, instill self-reliance and communicate effectively with target groups.
- Partially empowering communities by involving them in needs assessment, planning, beneficiary selection and program implementation, but keeping central government control over resource allocation
- Ensuring self-reliance:
- Seek local financial contributions to almost all interventions, so as to cut costs, involve communities, instill self-reliance, and increase the chances of sustainability
- International co-operations:
- Set up task forces involving UN agencies, NGOs and bilateral agencies to share technology and best practices
BEST PRACTICES:
- Thailand’s National Nutrition Program:
- Thailand has been much more successful in reducing protein-energy malnutrition (PEM), and iodine and vitamin A deficiency than most other countries in Asia
- Thailand’s approach to nutrition improvement has relied on empowering local communities
CONCLUSION:
- According to Global Nutrition Report 2015, investment in nutrition has a benefit cost ratio of 16:1 >> hence public spending to improve nutritional security has higher efficiency.
- It is critical to prevent under-nutrition as it compromises maternal and child health thereby undermining the learning outcomes in elementary education and hence affects labour productivity.
- With sustained prioritization, increased resource allocation, adopting comprehensive, coordinated and holistic approach with good governance and help of civil society, India has the potential to end malnutrition in all its forms and turn the ambition of the Sustainable Development Goals into a reality for everyone.
PRACTICE QUESTION:
Q. “Malnutrition is both a consequence as well as a cause of perpetuating poverty”. Analyse