Right to Health
2023 MAR 31
Mains >
Social justice > Health > Universal Healthcare
IN NEWS:
- Rajasthan assembly recently passed the Right to Health Bill. Once the bill is notified, Rajasthan would become the first state in India to guarantee right to healthcare for its residents.
- The law, which also provides for a social audit and grievance redress, gives every resident of the State the right to emergency treatment without paying a single paisa to any health-care institution, and specifies that private health-care institutions would be compensated for the charges incurred for such treatment.
RIGHT TO HEALTH:
- According to the World Health Organization (WHO), the right to health for all people means that everyone should have access to the health services they need, when and where they need them, without suffering financial hardship. No one should get sick and die just because they are poor, or because they cannot access the health services they need.
- Good health is also clearly determined by other basic human rights including access to safe drinking water and sanitation, nutritious foods, adequate housing, education and safe working conditions.
RIGHT TO HEALTH IN INDIA:
- Constitutional provisions:
- The Constitution of India does not expressly guarantee a fundamental right to health. However, there are multiple references in the Constitution to public health and on the role of the State in the provision of healthcare to citizens.
- The Directive Principles of State Policy:
- The Directive Principles of State Policy in Part IV of the India Constitution provide a basis for the right to health.
- Article 39 (E) directs the State to secure health of workers.
- Article 42 directs the State to just and humane conditions of work and maternity relief
- Article 47 casts a duty on the State to raise the nutrition levels and standard of living of people and to improve public health.
- Fundamental Right: Article 21
- Given no explicit recognition of the right to health or healthcare under the Constitution, the Supreme Court of India in Bandhua Mukti Morcha v Union of India & Ors. interpreted the right to health under Article 21 which guarantees the right to life.
- In State of Punjab & Ors. v Mohinder Singh Chawla the apex court reaffirmed that the right to health is fundamental to the right to life and should be put on record that the government had a constitutional obligation to provide health services.
- Role of Panchayats and Municipalities (Article 243G):
- The Constitution not only oblige the State to enhance public health, but also endows the Panchayats and Municipalities to strengthen public health under Article 243G (read with 11th Schedule, Entry 23).
- 15th Finance Commission:
- In September 2019, a High-Level Group on the health sector constituted under the 15th Finance Commission had recommended that the right to health be declared a fundamental right.
- It also put forward a recommendation to shift the subject of health from the State List to the Concurrent List.
THE IMPORTANCE OF RIGHT TO HEALTH:
- Breaks discriminatory structures that exist in healthcare:
- The right to equality guaranteed under Article 15 upholds non-discrimination on the basis religion, race, caste, gender, place of birth, etc. However, the dismal investment in public health for decades has made healthcare a privilege available to a few.
- The constitutional right to health is critical to breaking discriminatory structures that will otherwise continue to perpetuate inequality in all spheres of life, including education, opportunity, wealth, and social mobility.
- Improve the entire health ecosystem:
- By bringing in a law to give people healthcare as a right, the government would be strengthening people’s ability to demand better healthcare and also hold the government and healthcare workers accountable if it did not provide it.
- Special legislation and other mechanisms to strengthen healthcare:
- Constitutional right to health will pave the way for special legislation, capable institutions, increased budgets, medical training and research, wellness and prevention, and outreach of services; thereby strengthening the entire health ecosystem.
- For example, the right to education too had long been upheld as implicit to the right to life before the constitutional amendment that established it as fundamental in its own right. Now, the primary school enrolment rate is over 95 per cent, a target believed to be impossible 15 years ago.
- Reduce out of pocket expenditure:
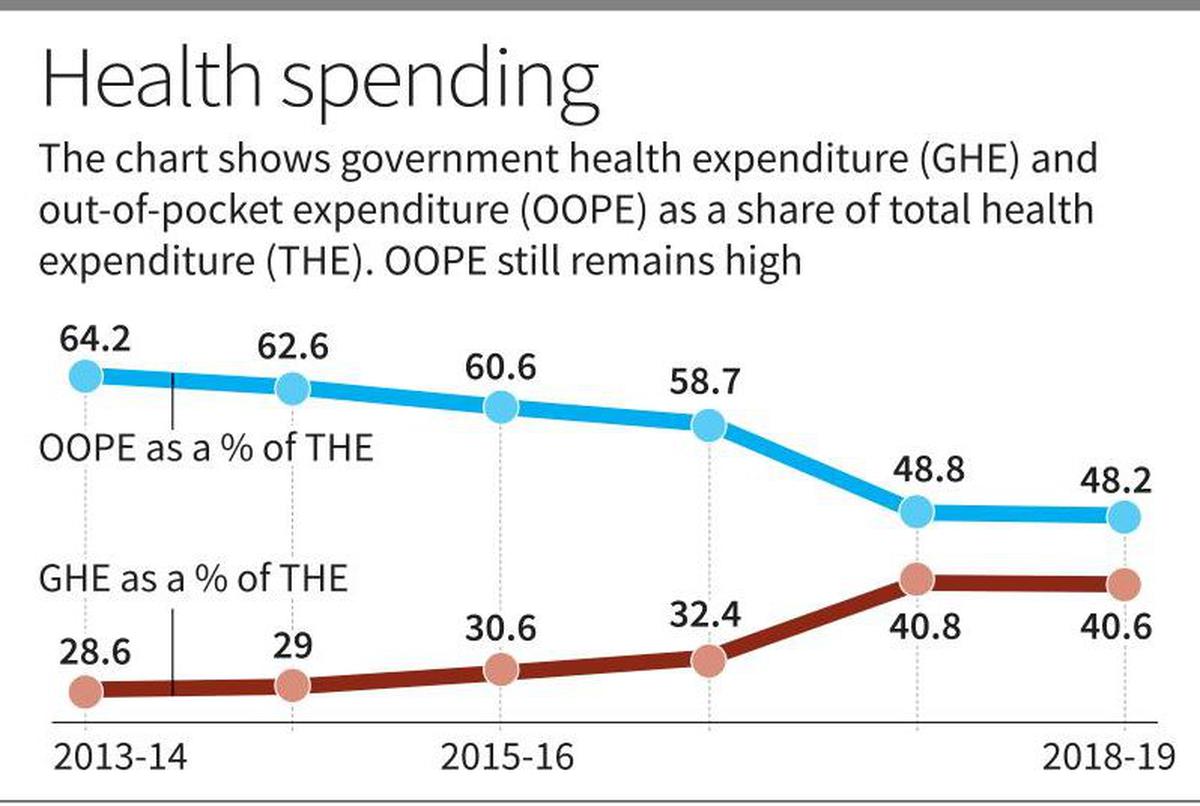
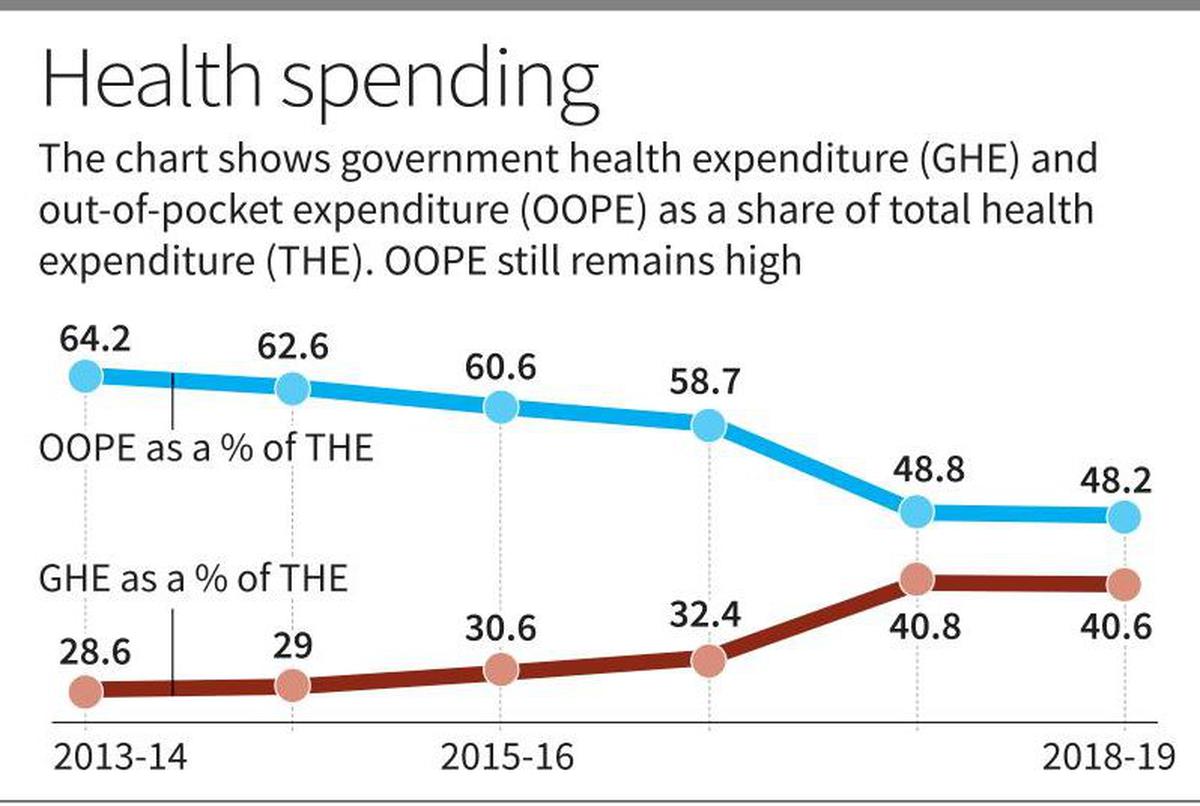
- According to the Economic Survey 2022-23, almost half of all health spending in India is still paid by patients themselves directly at the point of treatment. The Right to Health is an attempt to bring down out-of-pocket expenditure on health and boost public spending.
CHALLENGES:
- Lack of infrastructure:
- The healthcare ecosystem in India lacks basic infrastructure to cater to the demands of a large population.
- For example, India has only 8.5 beds for every 10,000 citizens.
- Insufficient human resource:
- Doctor to patient (1 per 1456 patients) and nurse to patient (1.7 per 1000 patients) ratios are much lower than WHO standards, which is 1/1000 in the case of doctor to patient ratio and 3/1000 in the case of nurses.
- Also, fake doctors (quacks) continue to be a major threat to Indian healthcare system.
- Low spending on health care:
- India’s public health spending as a share of GDP is very low (1.6 % of GDP)
- Among the BRICS nations, India’s public health spending as a share of GDP is the lowest. In the case of Brazil, it is 3.96 %, Russia is 3.16 %, South Africa (4.46%) and China (3.02%).
- Issues regarding compensation:
- Delay in reimbursement is a sticking point with healthcare providers. There are also complaints that the package rates fixed for various medical procedures/ treatment are not remunerative enough or do not cover the actual cost.
- High disease burden:
- India has a high burden of communicable and non-communicable diseases, such as tuberculosis, diabetes and malaria. Addressing these diseases requires significant investment in healthcare infrastructure and resources.
- Urban centric:
- Hospital infrastructure, especially secondary and tertiary care, are concentrated in urban areas. This affects the accessibility of rural population to healthcare facilities.
- Weak financial position of states:
- Many states in India have strained finances. Implementing right to health would increase the social expenditure and further increase the financial stress.
- Pushback from healthcare industry:
- As seen in Rajasthan, doctors and private hospitals oppose such efforts, owing to fear that it would lead to them being overburdened and the compensation being non-remunerative.
WAY FORWARD
- Need a fundamental shift in the approach:
- We need a fundamental shift in our approach to healthcare. Instead of viewing it as spending, we have to see it as a high-yield investment that can considerably cut down future out-of-pocket costs and also increase output.
- Coordination between the centre and states:
- On a crucial subject like health, there must be coordination between the centre and states without impeding cooperative federalism, an essential element of the Indian Constitution.
- More power and support to states:
- Lessons from the COVID 19 response by centre and states show that while smooth coordination between states and the centre is imperative, health needs to continue to be in the State List.
- Decentralisation of power and funds to states for boosting their respective public health systems is therefore imperative.
- Increase public investment:
- India needs to increase its investment in healthcare infrastructure and resources to at least 2.5 per cent of GDP by 2025.
CONCLUSION
- As the constitution of WHO states, "the enjoyment of the highest attainable standard of health is one of the fundamental rights of every human being without distinction of race, religion, political belief, economic or social condition".
SUCCESS STORIES:
1. SINGAPORE:
- Singapore’s health care financing system is underpinned by the belief that all stakeholders share responsibility for attaining sustainable universal health coverage. Singapore has a multipayer health care financing framework, known as the 3Ms, comprises the following programs:
- MediShield Life, a universal basic health care insurance, is mandatory for citizens and permanent residents and provides lifelong protection against large hospital bills and select costly outpatient treatments.
- MediSave, a national medical savings scheme, helps cover out-of-pocket payments. Personal and employer salary contributions to MediSave accounts are mandatory for all working citizens and permanent residents. These tax-exempt, interest-bearing (currently 4% to 5%) accounts can be used to pay for family members’ health care expenses.1
- MediFund is the government’s safety net for needy Singaporeans who cannot cover their out-of-pocket expenses, even with MediSave.
2.CANADA:
- Canada has a decentralized, universal, publicly funded health system called Canadian Medicare. Health care is funded and administered primarily by the country’s 13 provinces and territories.
- Each has its own insurance plan, and each receives cash assistance from the federal government on a per-capita basis. Benefits and delivery approaches vary.
- All citizens and permanent residents, however, receive medically necessary hospital and physician services free at the point of use.
PRACTICE QUESTION:
Q. Besides being a moral imperative of a Welfare State, right to health is a necessary precondition for sustainable development. Critically analyse.