Digital Healthcare in India
2023 JAN 11
Mains >
Social justice > Health > Health
IN NEWS:
- The National Health Authority (NHA) recently launched a Digital Health Incentive Scheme (DHIS) for digital health ecosystem stakeholders.
MORE ON NEWS:
- The scheme aims to boost digital health transactions in the country under the Ayushman Bharat Digital Mission (ABDM).
- The incentives under this scheme would be provided to hospitals and diagnostic labs and also to the providers of digital health solutions such as Hospital/ Health Management Information Systems and Laboratory Management Information Systems.
- Under the DHIS, the eligible health facilities and digital solutions companies shall be able to earn financial incentives of up to four crore rupees based on the number of digital health records they create and link to Ayushman Bharat Health Account, ABHA.
- This incentive can be availed by the hospitals and diagnostic labs registered with Ayushman Bharat Digital Mission’s Health Facility Registry and fulfilling the eligibility criterion specified under the scheme.
- The estimated initial financial outlay of the incentive scheme is Rs. 50 crores for a period of six months starting from 1st January 2023 onwards.
|
Ayushman Bharat Digital Mission (ABDM)
- The Ayushman Bharat Digital Mission (ABDM) aims to develop the backbone necessary to support the integrated digital health infrastructure of the country.
- ADBM is implemented by the National Health Authority (NHA) under the Ministry of Health and Family Welfare
- To read more about ABDM: https://ilearncana.com/details/Ayushman-Bharat-Digital-Mission/2513
|
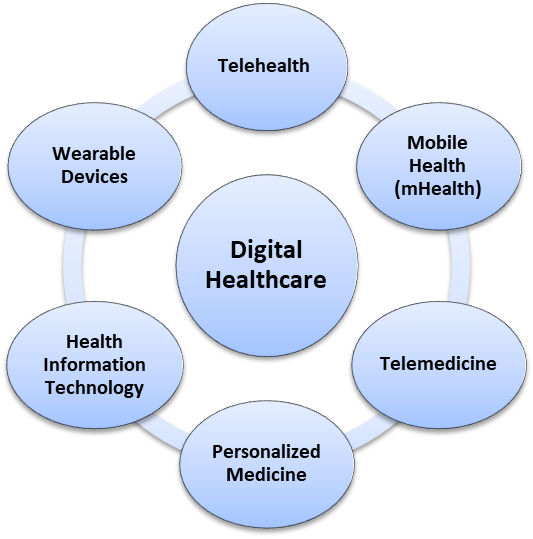
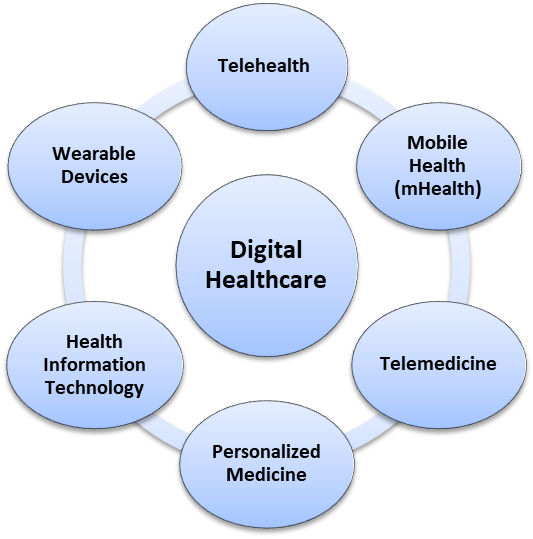
WHAT IS DIGITAL HEALTHCARE?
- Digital healthcare, or digital health, refers to the use of information and communications technologies in medicine and other health professions to manage illnesses and health risks and to promote wellness.
------------------------------------
BENEFITS OF DIGITAL HEALTHCARE:
- Improved access to quality healthcare:
- Digital health makes quality healthcare affordable and accessible, even in hard-to-reach areas.
- Through an internet connection, anyone can access health services and always be connected to a professional to resolve concerns.
- This will be beneficial for a country like India, where 70% of the population lives in rural areas while only 20% of the hospitals are located there.
- Prevention before treatment:
- Technologies that support digital health can help patients manage their health issues through regular monitoring of their symptoms.
- Digital health offers a tool that can help in the early detection of signs indicating disease development and progression before significant damage to the patient's health has occurred.
- For instance, smart watches have now transformed into clinically viable healthcare tools. Apple launched the Apple Heart Study app to monitor users’ heart rhythms and alert those who are experiencing atrial fibrillation.
- Make medicine more personalized for patients:
- Patients can use digital health technologies to manage and track their wellness-related activities.
- These technologies include the use of devices like smartphones, internet applications, and social networks that can help personalise treatment plans for patients based on their specific complaints and health parameters.
- Transparency in the patient-doctor relationship:
- Engaging in digital health systems can allow patients to connect with their healthcare providers more easily. In some cases, it can make the patients co-designers of their treatment plans.
- Direct, quick, and shared access to their health status can help patients develop a sense of partnership and improve their trust in the physician and treatment. It can also help to maintain transparency in the patient-doctor relationship.
- Reduces inefficiencies:
- Digital tools give healthcare providers a holistic view of the patient’s health through easy access to data.
- It can also allow patients to gain better control over their health, thereby reducing inefficiencies in patient management.
- Improve access:
- Digital health systems offer real-time opportunities to doctors to improve medical outcomes and treatment efficiency by providing quick access to the patient’s data in a format that can be interpreted easily with better clarity and accuracy.
- Reduce costs:
- Digital health would reduce the cost of overall treatments by supporting the patient’s ability to manage self-care through the apps that can monitor their health parameters.
INDIA'S OPPORTUNITIES IN DIGITAL HEALTHCARE:
- Existing public digital infrastructure:
- The current strong public digital infrastructure—including that related to Aadhaar, Unified Payments Interface and wide reach of the Internet and mobile phones (JAM trinity) —provides a strong platform for establishing the building blocks of ABDM.
- The existing ability to digitally identify people, doctors, and health facilities, facilitate electronic signatures, ensure non-repudiable contracts, make paperless payments, securely store digital records, and contact people provide opportunities to streamline healthcare information through digital management.
- Past experience:
- Ayushman Bharat—Pradhan Mantri Jan Arogya Yojana:
- Ayushman Bharat—Pradhan Mantri Jan Arogya Yojana (AB-PMJAY) has successfully used the available public digital infrastructure to provide end-to-end services through an information technology (IT) platform from identification of beneficiaries to their admission and treatment in hospitals to their discharge and paperless payment to hospitals.
- The experience of AB-PMJAY can be leveraged to expand the reach of digital health to all residents and develop an open and inter-operable health management system that empowers residents, healthcare providers, the Government and researchers.
- The effective use of digital healthcare in pandemic response :
- India leveraged information and communications technologies (ICTs) in health care during the COVID-19 pandemic.
- Digital health solutions played a crucial role in bridging the gap in healthcare delivery as systems moved online to accommodate contactless care.
- Some examples of digital public goods (DPG) developed during the pandemic include the Covid Vaccine Intelligence Network (CoWIN) and the Aarogya Setu application.
- CoWIN propelled India to adopt a completely digital approach to its vaccination strategy.
- Aarogya Setu provided real-time data on active cases and containment zones to help citizens assess risk in their areas.
- Also, telemedicine platforms saw a steep increase in user acquisitions, as 85 per cent of physicians used teleconsultations during the pandemic, underscoring the need to better incorporate cutting-edge digital technologies into healthcare services.
- Emerging technologies:
- Emerging technologies such as artificial intelligence, the internet of things (IoT), Blockchain and cloud computing provide additional opportunities for facilitating a more holistic digital health ecosystem, that can increase the equitable access to health services, improve health outcomes and reduce costs.
- Technical manpower:
- India can become a digital health leader, as India has been a frontrunner in IT and software and has the best technical manpower.
CHALLENGES AND CONCERNS:
- Privacy concerns:
- With India still lacking a law on data protection, the digital healthcare is expected to trigger privacy concerns in the days to come.
- The possibility of privacy being violated increases with the centralisation of all information.
- Even before the recent Data Protection Bill, the Government introduced The Digital Information Security in Healthcare Act (DISHA) 2018.DISHA was enacted to secure and standardize digital health information to maintain its privacy and confidentiality. While the purpose of this law is to encourage the pan-India adoption of e-health standards, it has not yet come into force.
- High initial cost:
- While technology helps smoothen processes and enhance patient experience, there is a cost attached.
- Investments have to be made upfront.
- For instance, in the immediate short run, Ayushman Bharat Digital Mission (ABDM) will increase administrative costs by about 20 per cent, due to the capital investment in hardware and software development, technical personnel and data entry servers.
- Lack of infrastructure:
- A large majority of facilities do not have the required physical infrastructure - electricity, accommodation, trained personnel.
- Operational challenges:
- Cards getting corrupted, servers being down, computers crashing or hanging, and power outages may seriously affect the functioning of digital healthcare.
- The inability to synchronise biometric data with ID cards has resulted in large-scale exclusions of the poor from welfare projects. Such a scenario is not inconceivable and in the case of health, may cause immense hardship to the most marginalised sections of our population.
- Shortcoming of using tele-consultation:
- In handling chronic diseases that necessitate continuity of care, tele-consultations have been problematic and cannot be substituted for actual physical examination.
- Continuity of care is central to good outcomes in patient management of chronic diseases.
- The one serious shortcoming of using tele-consultation for such management is the high attrition rate of doctors within the context of an overall shortage of doctors.
-
- For instance, in India, the doctor-patient ratio is 1 per 1456 patients, which is much lower than the WHO standard of 1/1000.
- Administrative hurdles:
- Health is a subject under the state list. This poses issues in ensuring coordination and uniformity across the country.
- There is no single authority responsible for public health that is legally empowered to issue guidelines and enforce compliance of the health standards.
- These administrative hurdles may affect the smooth functioning of the digital health care ecosystem in the country.
WAY FORWARD:
- Specific Data Protection Law:
- The Data Protection Rules is inadequate to anticipate and regulate the challenges posed by digital health.
- Though the newly introduced draft Digital Personal Data Protection Bill 2022 will aid in clarifying certain aspects of data protection measures to be extended to users of digital health interfaces, the governance of health data will require a more specific approach like the DISHA 2018.
- The adoption of a specific health data law or set of guidelines will aid in the development of a robust digital health ecosystem.
- Additionally, there is also a need for specific legislations to regulate telemedicine and online pharmacies.
- Increase health financing:
- The government should increase public expenditure on health to at least 3% of GDP, as the digital health ecosystem requires huge initial capital investments.
- The National Health Policy (NHP) 2017 had set a target of government expenditure on health at 2.5 % of the GDP by 2025 and had asked the states to spend at least 8% of their Budget on the health sector by 2020.
- A dedicated financial institution may also be established.
For extra reading: https://ilearncana.com/details/Healthcare-in-India/3832
PRACTICE QUESTION:
Q. Explain the key components of the Ayushman Bharat Digital Mission. Discuss the benefits and challenges associated with digitising the health sector in India?